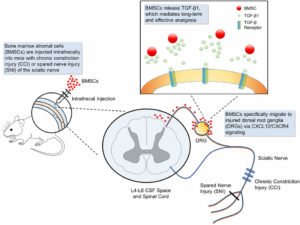
This review, although not very recent, examines the main experimental animal models of chronic pain, the basis of which, as is known, are those of neuroinflammation, and the effects on them of treatment with bone marrow-derived stem cells. Similarly to their use in other clinical fields, bone marrow-derived stem cells also exert an inflammation-modulating action here.
(Dott. Rosario Miranda)
<www.frontiersin.org/files/Articles/292133/fimmu-08-01014-HTML/image _m/fimmu-08-01014-g001.jpg>
Huh Y, Ji RR, Chen G. Neuroinflammation, Bone Marrow Stem Cells, and Chronic Pain. <pubmed.ncbi.nlm.nih.gov/28871264/> Front Immunol. 2017 Aug 21;8:1014.
Abstract
Current treatments for chronic pain, such as inflammatory pain, neuropathic pain, and cancer pain are insufficient and cause severe side effects. Mounting evidence suggests that neuroinflammation in the peripheral and central nervous system (PNS and CNS) plays a pivotal role in the genesis and maintenance of chronic pain. Characteristic features of neuroinflammation in chronic pain conditions include infiltration of immune cells into the PNS [e.g., the sciatic nerve and dorsal root ganglion (DRG)], activation of glial cells such as microglia and astrocytes in the CNS (spinal cord and brain), and production and secretion of pro-inflammatory cytokines and chemokines [TNF, interleukin (IL)-1β, IL-6, CCL2, and CXCL1]. Recent studies suggest that bone marrow stem cells or bone marrow stromal cells (BMSCs) produce powerful analgesic effects in animal models of inflammatory pain, neuropathic pain, and cancer pain. We recently demonstrated that intrathecal injection of BMSCs resulted in a long-term relief of neuropathic pain for several weeks after peripheral nerve injury. Strikingly, this analgesic effect is mediated by the anti-inflammatory cytokine transforming growth factor beta secreted from BMSCs. Additionally, BMSCs exhibit potent modulation of neuroinflammation, by inhibiting monocyte infiltration, glial activation, and cytokine/chemokine production in the DRG and spinal cord. Thus, BMSCs control chronic pain by regulation of neuroinflammation in the PNS and CNS via paracrine signaling. In this review, we discuss the similar results from different laboratories of remarkable anti-nociceptive efficacy of BMSCs in animal and clinical studies. We also discuss the mechanisms by which BMSCs control neuroinflammation and chronic pain and how these cells specifically migrate to damaged tissues.
Keywords:
bone marrow stem cells; chronic pain; neuroinflammation; transforming growth factor beta; treatment.